6 Easy Steps to improve your Gut Health: The Foundation of Your Overall Wellness
What’s Gut Health? Have you ever experienced that “gut feeling” when something doesn’t seem right? This common expression might be more scientifically accurate than you realize. Your gut health plays a critical role in your overall well-being, influencing everything from your immune system to your mental health. This comprehensive guide explores the fascinating world of gut health and provides actionable insights to optimize your digestive wellness.
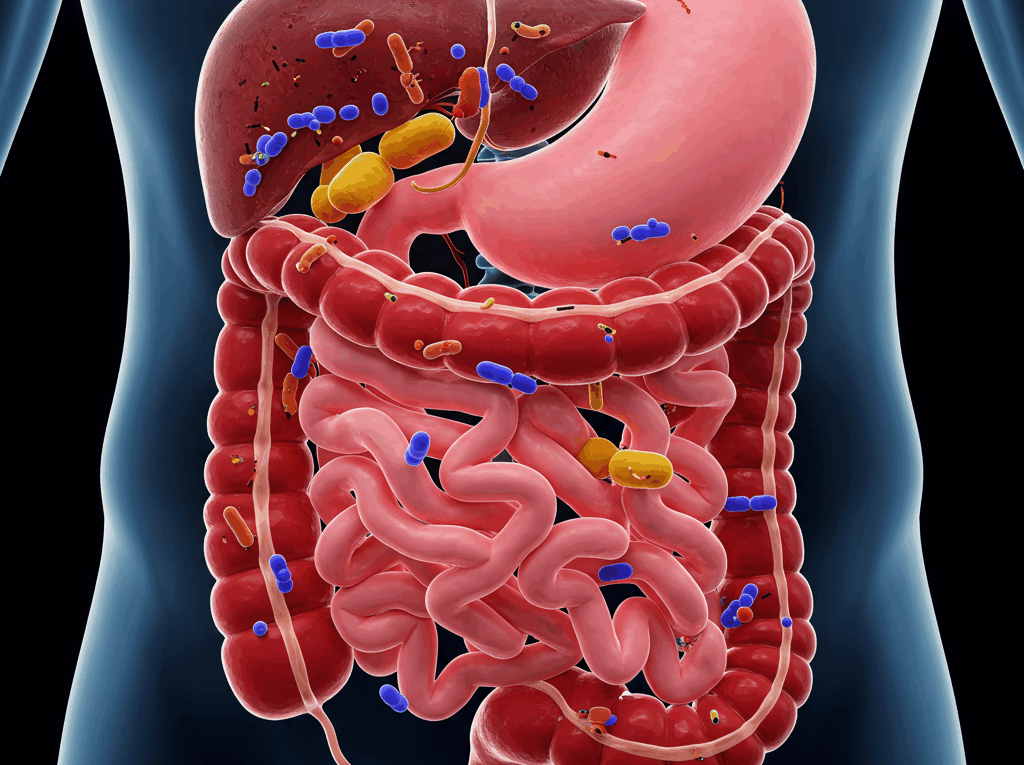
Understanding the Gut Microbiome: Your Internal Ecosystem
The human gut contains trillions of microorganisms collectively known as the gut microbiome. This complex ecosystem includes bacteria, viruses, fungi, and other microscopic organisms that coexist within your digestive tract. A healthy adult carries approximately 3-5 pounds of these microorganisms—roughly the weight of a small laptop!
Research shows that your gut hosts over 1,000 species of bacteria alone, with each person having a unique microbial fingerprint. These microorganisms aren’t merely passive inhabitants; they actively participate in numerous bodily functions:
- Breaking down food components your body can’t digest on its own
- Producing essential vitamins (including B vitamins and vitamin K)
- Training your immune system to recognize harmful pathogens
- Creating neurotransmitters that affect mood and cognitive function
- Protecting against harmful bacteria that cause illness
When your gut microbiome exists in a balanced state—known as eubiosis—these functions proceed optimally. However, when the balance tips toward harmful microorganisms—a condition called dysbiosis—numerous health problems can emerge.
You can also like this content about gut health: “Follow your gut…”
The Gut-Brain Connection: How Your Digestive System Affects Your Mood
One of the most fascinating discoveries in recent medical research is the powerful bidirectional communication pathway between your gut and your brain, often called the “gut-brain axis.” This connection explains why digestive issues often coincide with mental health challenges.
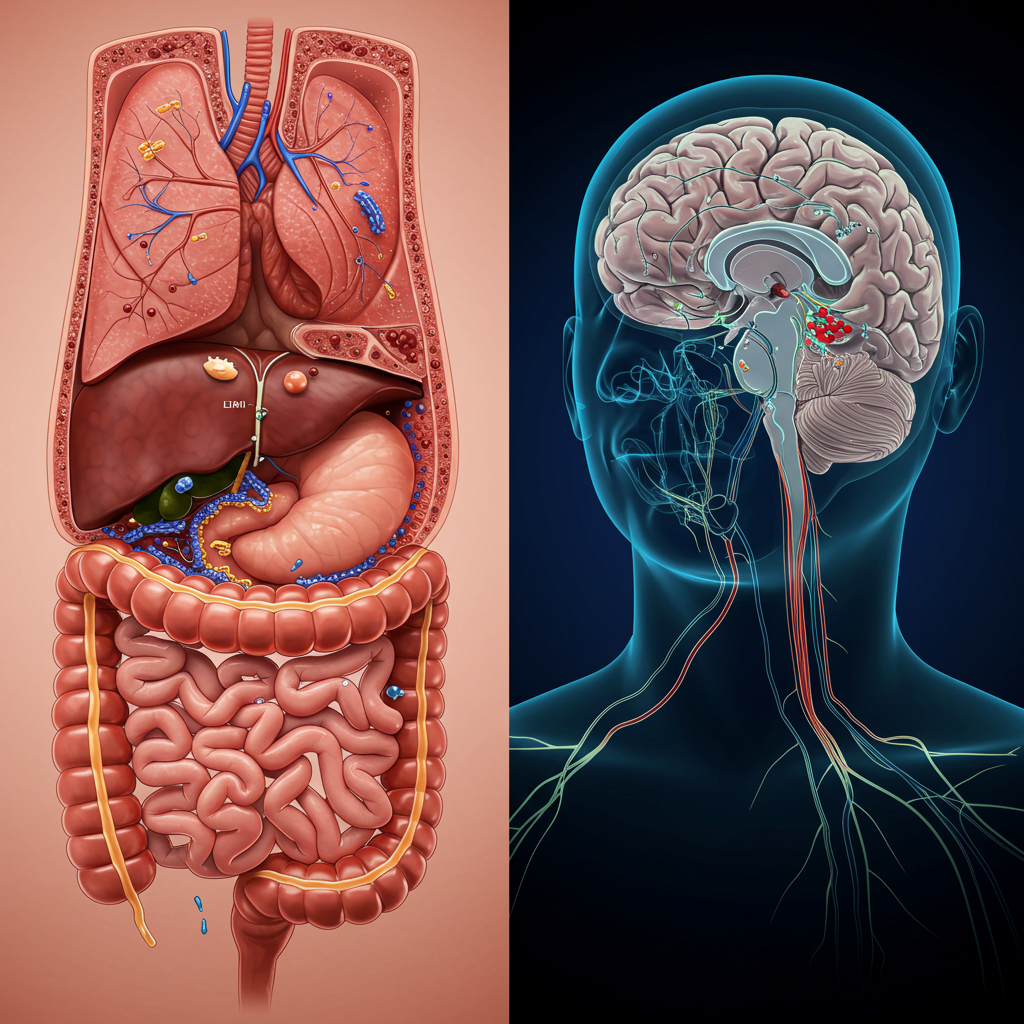
Your gut produces approximately 95% of your body’s serotonin, a neurotransmitter known for regulating mood, happiness, and anxiety. This explains why researchers have found strong correlations between gut health and mental health conditions:
- People with irritable bowel syndrome (IBS) are more likely to experience anxiety and depression
- Certain probiotic strains have demonstrated positive effects on mood disorders
- Stress can directly alter gut permeability and microbial composition
- Inflammatory markers from poor gut health can cross the blood-brain barrier and influence brain function
Dr. Michael Gershon, a pioneer in gut-brain research and author of “The Second Brain,” explains: “The gut has a mind of its own, the enteric nervous system. It’s a collection of neurons in the gastrointestinal tract that constitutes the ‘brain of the gut’ and can function independently of the central nervous system.”
You can read more studies about gut-brain here: Mind-gut connection.
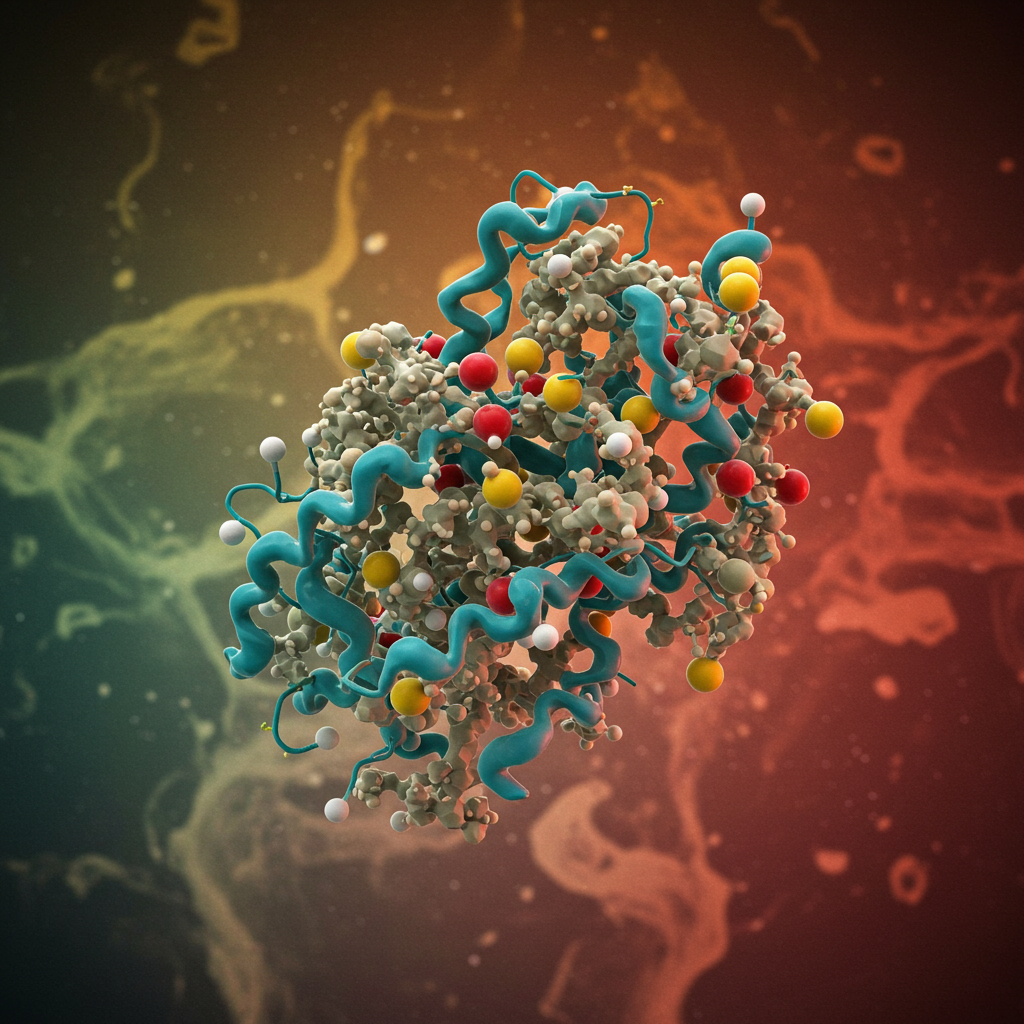
Probiotics and Prebiotics: Nurturing Your Internal Garden
Probiotics: The Beneficial Bacteria
Probiotics are live beneficial bacteria that, when consumed in adequate amounts, provide health benefits. These “good” bacteria help maintain the delicate balance of your gut ecosystem. Common probiotic strains include:

- Lactobacillus: Found in yogurt and fermented foods, these bacteria help break down lactose and other sugars.
- Bifidobacterium: These populate the colon and help prevent harmful bacteria from establishing themselves.
- Saccharomyces boulardii: A beneficial yeast that helps combat diarrhea and other digestive issues.
Research published in the Journal of Clinical Gastroenterology shows that specific probiotic strains can help with conditions including:
- Antibiotic-associated diarrhea (reduced by up to 60%)
- Irritable bowel syndrome symptoms (improved in approximately 70% of patients)
- Inflammatory bowel diseases like Crohn’s and ulcerative colitis (reduced inflammation markers)
- Certain allergic reactions (decreased severity in about 40% of cases)
Prebiotics: Fuel for Your Beneficial Bacteria
While probiotics introduce beneficial bacteria, prebiotics feed them. These specialized plant fibers aren’t digested by your body but instead serve as food for your beneficial gut bacteria. Common prebiotic sources include:
- Chicory root (contains up to 65% inulin)
- Jerusalem artichokes (rich in fructooligosaccharides)
- Dandelion greens (contain high levels of inulin and oligofructose)
- Garlic and onions (abundant in fructooligosaccharides)
- Bananas (especially slightly underripe ones containing resistant starch)
- Oats (contain beta-glucan fibers)

When prebiotics are fermented by gut bacteria, they produce short-chain fatty acids (SCFAs) like butyrate, propionate, and acetate. These compounds:
- Provide energy for colon cells
- Reduce inflammation
- Strengthen the gut barrier
- Signal to the brain and immune system
You can read more here: “Role of the gut microbiota…”
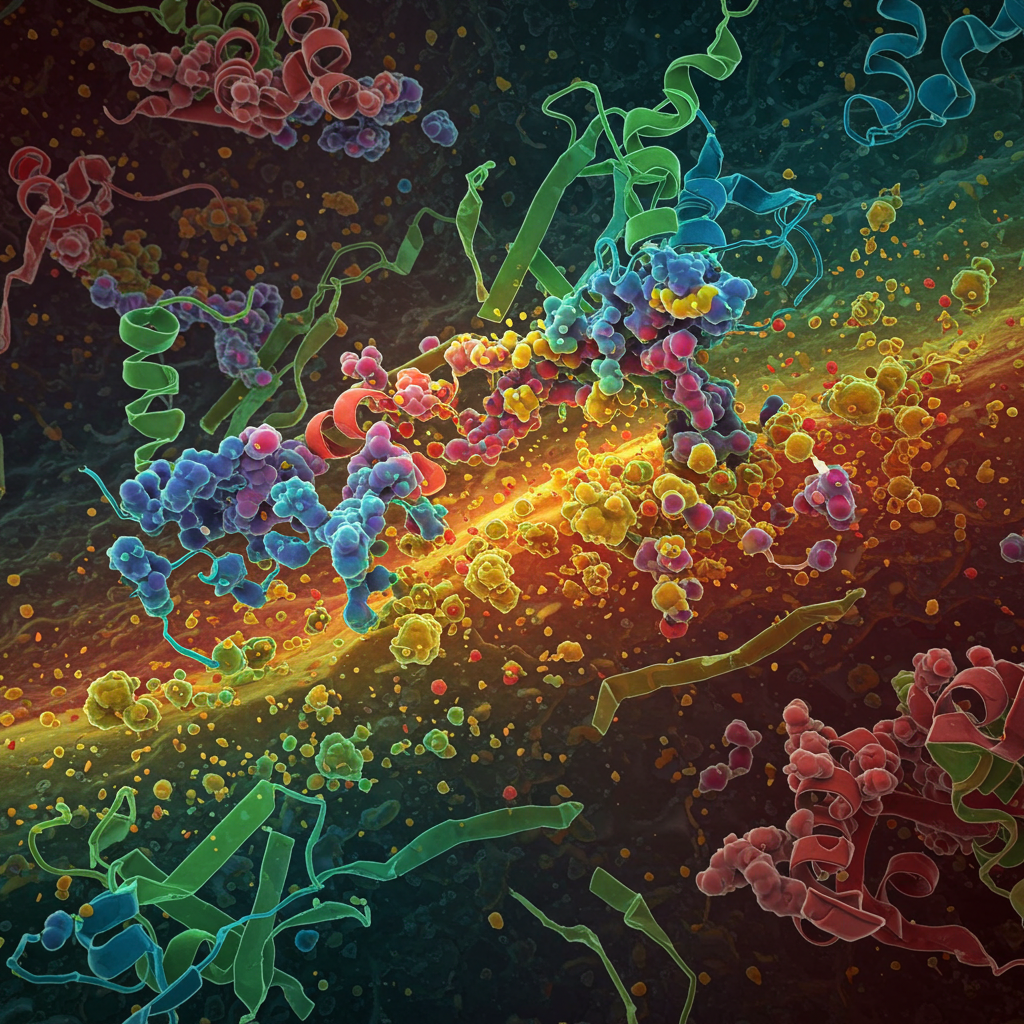
Digestive Enzymes: The Chemical Catalysts of Gut Health
Digestive enzymes are specialized proteins that break down food into smaller, absorbable components. Without sufficient digestive enzymes, even the healthiest diet can’t properly nourish your body. Key digestive enzymes include:
- Amylase: Breaks down complex carbohydrates into simple sugars
- Protease: Converts proteins into amino acids
- Lipase: Transforms fats into fatty acids and glycerol
- Lactase: Digests lactose (milk sugar)
- Cellulase: Helps break down plant cell walls and fibers
As we age, our natural enzyme production tends to decrease. Factors like chronic stress, genetic predispositions, and certain medications can further reduce enzyme levels. Signs of insufficient digestive enzymes include:
- Bloating shortly after meals
- Feeling uncomfortably full after eating small amounts
- Undigested food in stool
- Floating stools (indicating fat malabsorption)
- Nutrient deficiencies despite adequate intake
Dr. Elizabeth Lipski, author of “Digestive Wellness,” notes: “Digestive enzymes are like the workers in a factory assembly line, breaking down food so we can extract nutrients. Without enough enzymes, this process becomes inefficient, leading to both digestive symptoms and reduced nutrient availability.”
Leaky Gut Syndrome: When Your Intestinal Barrier Breaks Down
The lining of your intestines serves as a selective barrier, allowing nutrients to enter your bloodstream while keeping harmful substances out. This barrier consists of a single layer of cells held together by tight junctions—essentially the “security system” of your gut.
When these tight junctions become compromised, a condition known as increased intestinal permeability or “leaky gut syndrome” can develop. This allows partially digested food particles, toxins, and bacteria to leak into your bloodstream, potentially triggering widespread inflammation and immune responses.
Factors that can contribute to leaky gut include:
- Chronic stress (increases cortisol, which weakens intestinal junctions)
- Poor diet (especially high in processed foods and low in fiber)
- Excessive alcohol consumption
- Certain medications (particularly NSAIDs and antibiotics)
- Environmental toxins
- Chronic infections
Research published in the journal Frontiers in Immunology has linked increased intestinal permeability to numerous health conditions, including:
- Autoimmune disorders like type 1 diabetes and multiple sclerosis
- Inflammatory bowel diseases
- Food allergies and sensitivities
- Chronic fatigue syndrome
- Mood disorders and neurodegenerative conditions
The Gut-Immunity Connection: How Digestive Health Strengthens Your Defenses
Approximately 70-80% of your immune tissue resides in your digestive system, primarily in the form of gut-associated lymphoid tissue (GALT). This makes your gut the largest immune organ in your body. When your gut health is compromised, your entire immune system suffers.
Your gut microbiome educates your immune cells about which substances are harmless and which are potential threats. This training begins at birth and continues throughout life, with dietary choices significantly influencing immune development.
Studies show that individuals with diverse, balanced gut microbiomes typically experience:
- Fewer respiratory infections (reduced by up to 30% in some studies)
- Shorter duration of illness when infections do occur
- Lower rates of allergic reactions
- Reduced inflammation markers throughout the body
- Better vaccine responses
Dr. Emeran Mayer, gastroenterologist and author of “The Mind-Gut Connection,” states: “The immune system and the gut microbiome have co-evolved for millennia. Our modern lifestyles—including processed foods, overuse of antibiotics, and chronic stress—have disrupted this ancient relationship, contributing to the rise in immune-related disorders.”
Practical Strategies to Improve Your Gut Health
1. Diversify Your Diet with Fiber-Rich Foods
Dietary fiber serves as fuel for beneficial gut bacteria. Most Americans consume only about 15 grams of fiber daily, far below the recommended 25-38 grams. To increase your fiber intake:
- Aim for 8-10 servings of fruits and vegetables daily
- Include legumes like lentils, chickpeas, and beans several times weekly
- Choose whole grains over refined options
- Snack on nuts and seeds
A study in the American Journal of Clinical Nutrition found that participants who increased their fiber intake by just 6 grams per day experienced a 21% increase in beneficial gut bacteria within two weeks.
2. Incorporate Fermented Foods
Fermented foods naturally contain probiotics and have been used across cultures for thousands of years. Options include:
- Yogurt with live active cultures
- Kefir (containing up to 50 strains of beneficial bacteria)
- Sauerkraut (unpasteurized)
- Kimchi
- Kombucha
- Miso
- Tempeh
Research from Stanford University showed that consuming fermented foods increased microbial diversity and reduced inflammatory markers more effectively than simply adding fiber.
3. Consider Targeted Probiotic Supplements
While food sources are ideal, quality probiotic supplements can provide therapeutic doses of specific bacterial strains. When choosing a probiotic:
- Look for products with multiple strains
- Check for colony-forming units (CFUs) in the billions
- Ensure the product has proper storage requirements and guarantees viability through expiration
- Consider strain-specific benefits for your particular health concerns
4. Manage Stress Effectively
Chronic stress directly impacts gut function through the gut-brain axis. Effective stress management techniques include:
- Regular meditation (shown to reduce intestinal permeability in research studies)
- Deep breathing exercises (activates the parasympathetic “rest and digest” nervous system)
- Adequate sleep (7-9 hours for most adults)
- Regular physical activity (moderate exercise improves gut transit time and microbial diversity)
- Time in nature (reduces stress hormones and inflammation)
5. Avoid Overuse of Antibiotics and Other Gut-Disrupting Medications
While sometimes necessary, antibiotics can devastate your gut microbiome. When prescribed antibiotics:
- Take them exactly as directed
- Consider probiotic supplementation during and after treatment (separated by at least 2 hours)
- Focus on prebiotic-rich foods to help rebuild beneficial populations
Other medications that can impact gut health include proton pump inhibitors, NSAIDs, and certain antidepressants. Always discuss potential gut effects with your healthcare provider.
6. Stay Properly Hydrated
Water is essential for maintaining the mucus layer that protects your intestinal lining and supports proper digestion. Aim for:
- Approximately 2-3 liters daily for women
- Approximately 3-4 liters daily for men
- More during exercise, hot weather, or illness
Signs of adequate hydration include light yellow urine and regular bowel movements.
The Future of Gut Health Research
The science of gut health continues to evolve rapidly. Exciting areas of current research include:

- Personalized probiotics: Custom-formulated based on your unique microbiome composition
- Fecal microbiota transplantation: Already successful for certain conditions like C. difficile infection
- Psychobiotics: Specific probiotic strains that may help treat anxiety and depression
- Microbiome testing: Becoming more accessible and actionable for consumers
- Targeted prebiotics: Designed to feed specific beneficial bacterial strains
Frequently Asked Questions About Gut Health
What are the most common signs of poor gut health?
Common indicators of compromised gut health include bloating, gas, diarrhea, constipation, heartburn, and abdominal pain. However, signs can extend beyond your digestive tract. Unexplained fatigue, skin issues like eczema, food intolerances, autoimmune responses, and even mood disorders like anxiety or depression can all stem from gut imbalances. If you’re experiencing multiple symptoms, particularly after eating certain foods, consider consulting with a healthcare provider who specializes in digestive health.
How long does it take to improve gut health?
Gut health improvement is a gradual process that varies by individual. Many people notice reduced bloating and digestive discomfort within 2-3 weeks of dietary changes. More substantial improvements in energy, mental clarity, and overall well-being typically emerge after 4-6 weeks of consistent gut-supportive practices. Deeper healing of the gut lining may take 3-6 months or longer, especially if addressing long-standing issues like leaky gut syndrome. Consistency with diet, stress management, and supportive supplements yields the best results.
Can gut health affect my weight?
Yes, research increasingly shows that gut microbiome composition significantly impacts weight management. Specific bacterial populations can influence how much energy is extracted from food, hormone regulation (including those controlling hunger and satiety), and even fat storage. Studies have found that individuals with obesity often have different gut bacterial profiles than those at a healthy weight. Improving gut health through fiber-rich foods, fermented products, and reduced processed food intake may support weight management goals as part of a comprehensive approach.
Are all probiotics the same?
No, probiotics differ significantly in their effects and benefits. They vary by genus (like Lactobacillus or Bifidobacterium), species, and strain. Each probiotic strain has unique properties and potential health benefits. For example, Lactobacillus acidophilus may help with lactose digestion, while Bifidobacterium longum might better support immune function. When choosing probiotics, look for products that identify specific strains and their researched benefits rather than just listing general categories. Working with a knowledgeable healthcare provider can help you select the most appropriate probiotic for your specific health concerns.
Does stress really affect gut health?
Absolutely. The gut-brain axis provides a direct communication pathway between your digestive system and central nervous system. When you experience stress, your body releases cortisol and other stress hormones that can alter gut motility, reduce beneficial bacteria, increase intestinal permeability (leaky gut), and trigger inflammation. Many people notice digestive symptoms during stressful periods—this isn’t coincidental but reflects this powerful connection. Incorporating stress management techniques like meditation, deep breathing, adequate sleep, and regular exercise can significantly improve gut function.
Can children have gut health issues?
Yes, children can experience gut health problems, and early gut microbiome development is crucial for lifelong health. Factors that influence a child’s gut health include birth method (vaginal vs. cesarean), breastfeeding duration, antibiotic exposure, and diet diversity. Common signs of gut issues in children include recurring tummy aches, irregular bowel movements, food sensitivities, eczema, and frequent illnesses. Supporting children’s gut health through fiber-rich whole foods, limited processed foods and sugars, and age-appropriate probiotics can help establish healthy digestive patterns that benefit them throughout life.
What foods should I avoid for better gut health?
While individual sensitivities vary, certain foods commonly disrupt gut health for many people:
- Highly processed foods with artificial additives and preservatives
- Excessive refined sugar, which can feed harmful bacteria
- Industrial seed oils high in omega-6 fatty acids (like soybean and corn oil)
- Conventional dairy products, particularly for those with lactose intolerance
- Gluten-containing grains, especially for those with sensitivity or celiac disease
- Alcohol, which can damage the intestinal lining and alter the microbiome
- Artificial sweeteners, which may disrupt beneficial bacterial populations
Consider keeping a food journal to identify your personal triggers rather than eliminating food groups unnecessarily.
Should everyone take digestive enzymes?
Not necessarily. While digestive enzymes can benefit people with specific conditions like pancreatic insufficiency, age-related enzyme decline, or certain digestive disorders, healthy individuals typically produce adequate enzymes naturally. Before supplementing, try improving your natural enzyme production through proper eating habits: thoroughly chewing food, not drinking excessive liquids with meals, managing stress, and including naturally enzyme-rich foods like pineapple (containing bromelain) and papaya (containing papain). If you consistently experience symptoms like bloating after meals or undigested food in stool, consult a healthcare provider about whether enzyme supplementation might help.
How does gut health relate to autoimmune conditions?
The connection between gut health and autoimmunity is substantial. Approximately 70-80% of your immune tissue resides in your gut, and intestinal barrier integrity plays a crucial role in preventing inappropriate immune responses. When the gut barrier becomes compromised (leaky gut), partially digested food particles and microbes can enter the bloodstream, potentially triggering systemic inflammation and confusing the immune system. This process, called molecular mimicry, may lead the immune system to attack the body’s own tissues that resemble these particles. Many functional medicine approaches to autoimmune conditions focus on healing the gut as a fundamental step in managing these disorders.
Can improving gut health help with skin problems?
Yes, there’s a well-established gut-skin axis. Skin conditions like acne, rosacea, eczema, and psoriasis often improve when gut health is addressed. Inflammation originating in the gut can manifest on the skin, and certain gut bacterial imbalances are associated with specific skin disorders. Additionally, the gut microbiome influences how your body processes hormones that affect skin health. Many dermatologists now recognize the connection and recommend probiotics, omega-3 fatty acids, and anti-inflammatory diets alongside traditional skin treatments. For persistent skin issues, investigating and addressing underlying gut imbalances may provide substantial relief.
Conclusion: Your Gut Health Journey
The road to optimal gut health is not a quick fix but rather a lifestyle approach that incorporates dietary choices, stress management, mindful medication use, and sometimes targeted supplementation. By nurturing your internal ecosystem, you’re laying the foundation for overall wellness that extends far beyond digestive comfort.
Remember that gut health improvements often follow a pattern:
- Reduced bloating and digestive discomfort (often within days)
- Improved energy and clearer thinking (typically within weeks)
- Enhanced immune function and mood stability (usually within months)
- Long-term resilience against chronic diseases (over years)
As Hippocrates wisely stated over 2,000 years ago, “All disease begins in the gut.” Modern science continues to affirm this ancient wisdom, revealing the gut as not just a digestive organ but a cornerstone of physical and mental health.
If you want to read all the posts, click here: Vita Hub