3 Symptoms of Prostatitis and How Breaking Free from Pain Forever
Prostatitis affects millions of men worldwide, yet many suffer in silence, unaware that effective solutions exist, so Have you ever experienced that burning sensation during urination that makes you dread every bathroom visit? Or felt that persistent pelvic pain that seems to control your entire day? You’re not alone in this struggle.
This comprehensive guide will walk you through everything you need to know about prostatitis, from understanding its root causes to discovering natural treatment approaches that can transform your quality of life. Whether you’re dealing with acute symptoms or chronic discomfort, the information ahead could be the key to reclaiming your health and confidence.
What Exactly Is Prostatitis?
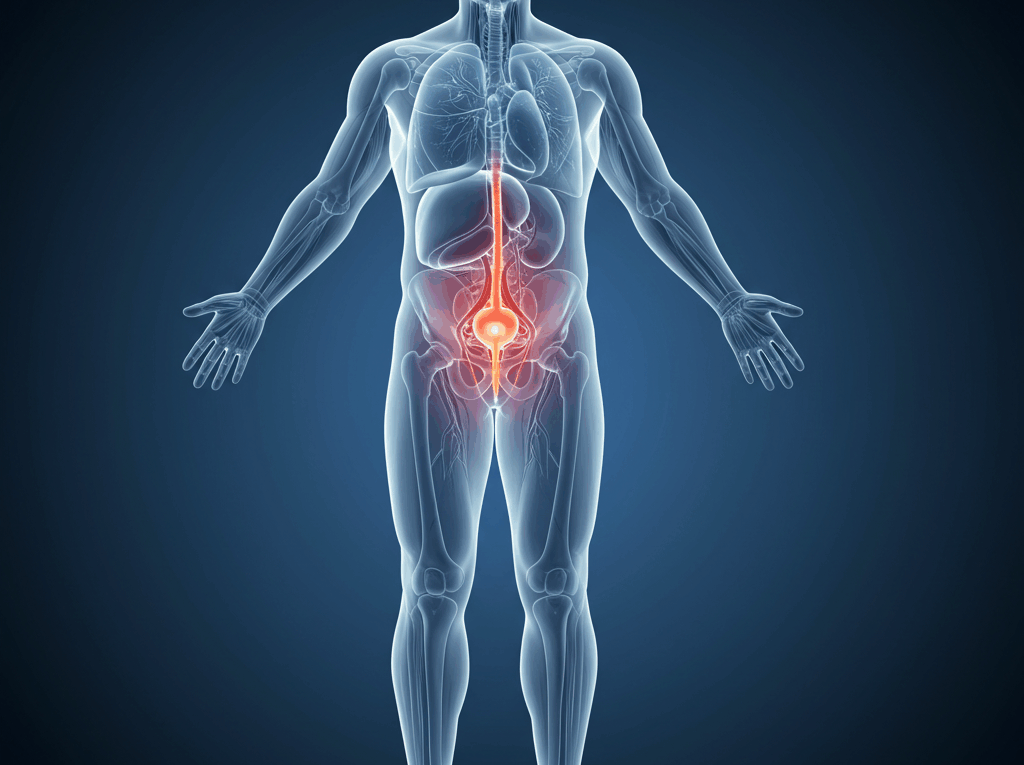
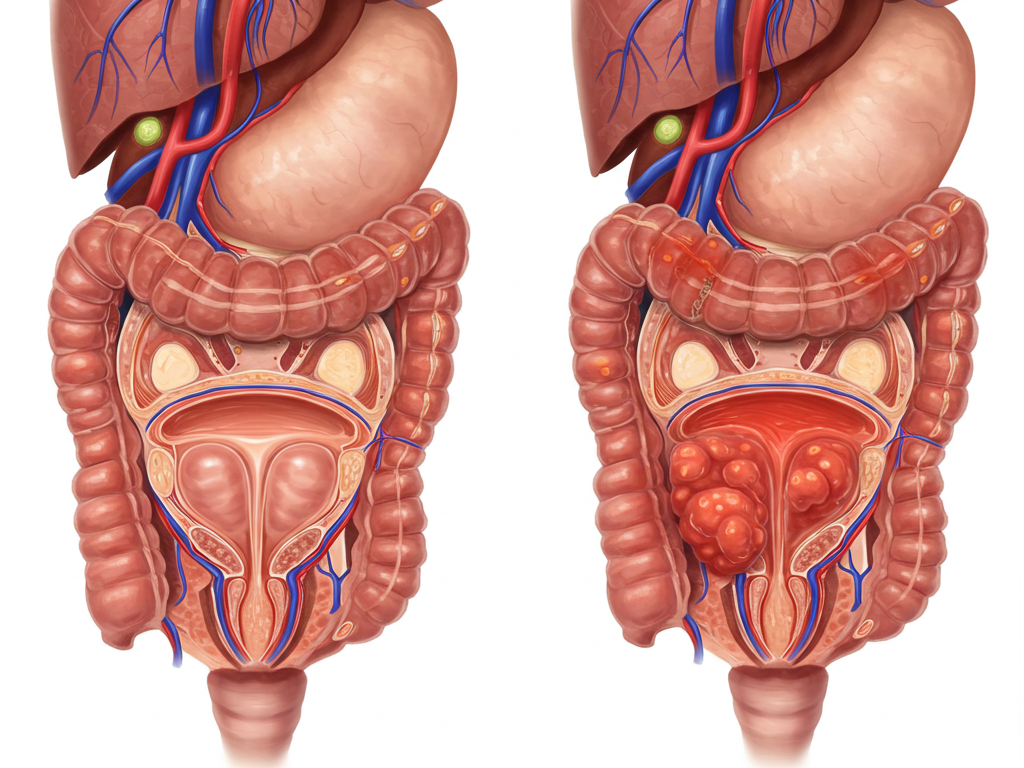
Prostatitis is inflammation of the prostate gland, a walnut-sized organ that plays a crucial role in male reproductive health. Think of your prostate as a security guard for your urinary system – when it becomes inflamed, it can’t perform its duties effectively, leading to a cascade of uncomfortable symptoms.
Understanding Your Prostate Gland
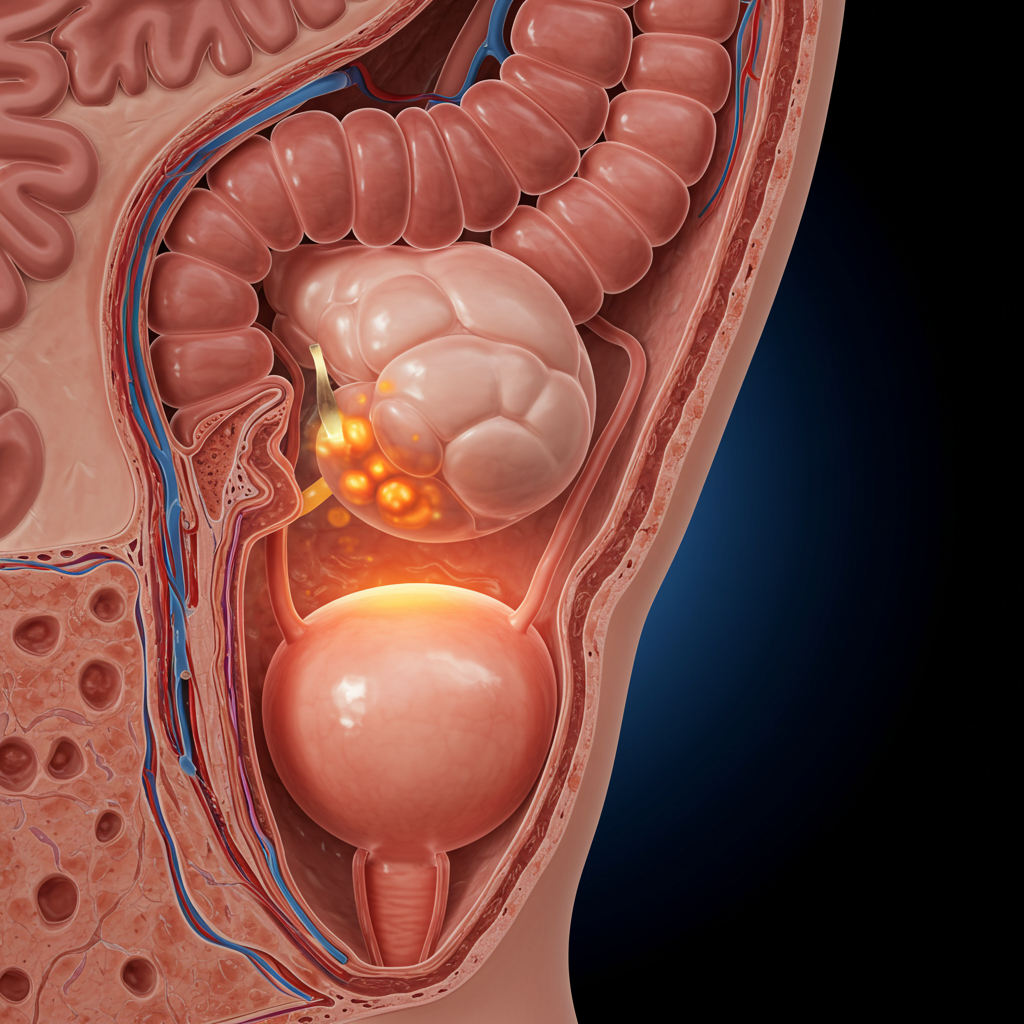
Your prostate gland sits just below your bladder and surrounds your urethra like a protective sleeve. It produces prostatic fluid, which nourishes and protects sperm during ejaculation. When this gland becomes inflamed, it can swell and press against surrounding tissues, causing the painful symptoms associated with prostatitis.
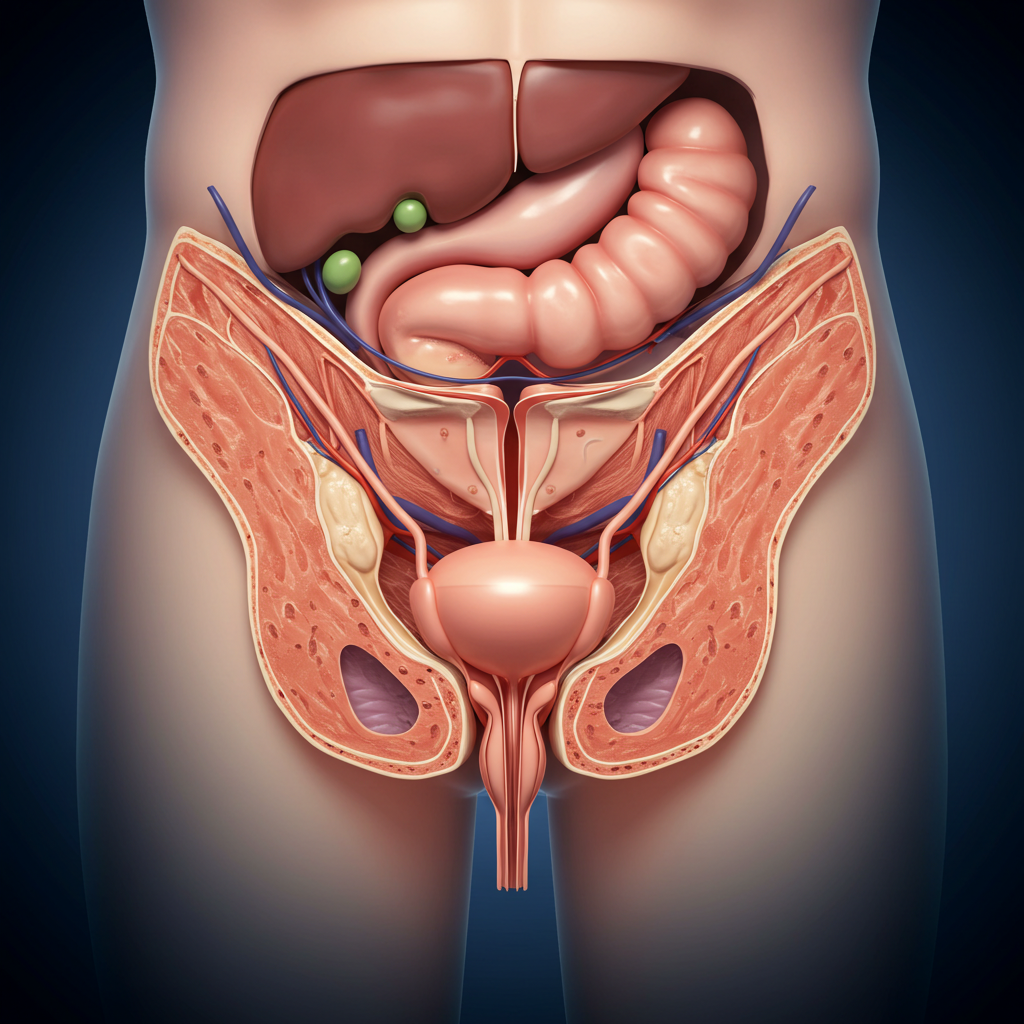
The prostate contains smooth muscle fibers that help expel semen during ejaculation. When inflammation occurs, these muscles can become tense and spastic, contributing to pelvic pain and urinary difficulties that many men experience.
You can read more here.
The Four Types of Prostatitis
Medical professionals classify prostatitis into four distinct categories, each requiring different treatment approaches:
Acute bacterial prostatitis represents the most severe form, typically caused by bacterial infections that develop suddenly. Men with this condition often experience fever, chills, and severe pelvic pain that requires immediate medical attention.
Chronic bacterial prostatitis develops more gradually and persists for extended periods. While less intense than the acute form, it can significantly impact daily life and requires sustained treatment approaches.
Chronic pelvic pain syndrome accounts for approximately 90% of all prostatitis cases. This non-bacterial form remains the most challenging to diagnose and treat, as its exact causes often remain unclear.
Asymptomatic inflammatory prostatitis produces no noticeable symptoms but shows signs of inflammation during medical examinations. Many men remain unaware they have this condition until routine testing reveals its presence.
Read more about how to treat with natural supplements in this article: The best prostate health supplements…
Recognizing the Warning Signs
Understanding prostatitis symptoms can help you seek appropriate treatment before the condition worsens. Many men initially dismiss these signs as temporary discomfort, allowing the problem to progress unnecessarily.
You can read more about it here.
Physical Symptoms You Can’t Ignore
The most common physical manifestations of prostatitis include burning or painful urination that can make every bathroom visit an ordeal. You might notice increased urinary frequency, especially during nighttime hours, disrupting your sleep patterns and leaving you exhausted.

Pelvic pain often radiates to various areas, including the lower back, groin, and even the tip of the penis. This pain can range from a dull ache to sharp, stabbing sensations that interfere with sitting, walking, or even lying down comfortably.
Sexual function may also be affected, with some men experiencing painful ejaculation or decreased libido. These symptoms can create a vicious cycle where physical discomfort leads to anxiety about sexual performance, further exacerbating the condition.
You can read about how to reduce these symptoms in this article: Click here
Mental Health Impact
The psychological effects of prostatitis often receive less attention but can be equally devastating. Chronic pain and urinary symptoms can lead to anxiety, depression, and social withdrawal as men struggle to manage their condition while maintaining normal activities.
Sleep disruption from frequent nighttime urination creates additional stress on your body and mind. When you’re constantly tired and in pain, it becomes challenging to maintain positive relationships and perform effectively at work or in social situations.
Sleep Disruption Patterns
Nocturia, or frequent nighttime urination, affects nearly 80% of men with prostatitis. This symptom can wake you multiple times per night, preventing the deep, restorative sleep your body needs to heal and function optimally.
The frustration of interrupted sleep often compounds other prostatitis symptoms, creating a cycle where poor sleep worsens inflammation, and increased inflammation further disrupts sleep quality.
Relationship Challenges
Prostatitis can strain intimate relationships as sexual symptoms and chronic pain affect both partners. Open communication becomes essential, yet many men feel embarrassed discussing these sensitive health issues with their loved ones.
The condition may also impact social activities and work performance, as unpredictable symptoms can make it difficult to commit to plans or maintain consistent productivity levels.
Root Causes That Trigger Prostatitis
Understanding what triggers prostatitis can help you address the underlying issues rather than merely managing symptoms. While the exact causes aren’t always clear, several factors consistently contribute to prostate inflammation.
Bacterial Infections
Bacterial prostatitis typically results from common bacteria like E. coli that normally inhabit your digestive system. These bacteria can reach your prostate through various pathways, including backward flow of infected urine or direct spread from nearby infected tissues.
Urinary tract infections that aren’t properly treated can ascend to the prostate, establishing persistent bacterial colonies that resist standard antibiotic treatments. This is why early intervention for UTIs is crucial for preventing more serious prostate complications.
Sexual activity can sometimes introduce bacteria into the urinary tract, particularly if proper hygiene isn’t maintained. However, it’s important to note that prostatitis isn’t considered a sexually transmitted disease, though certain practices may increase infection risk.
Stress and Lifestyle Factors
Chronic stress plays a significant role in prostatitis development and persistence. When you’re under constant stress, your immune system becomes compromised, making you more susceptible to infections and inflammatory conditions.
High-stress levels also increase muscle tension throughout your body, including the pelvic floor muscles that support your prostate. This tension can restrict blood flow and contribute to the pain and dysfunction associated with prostatitis.
Diet-Related Triggers
Certain foods can irritate your prostate and worsen prostatitis symptoms. Spicy foods, caffeine, alcohol, and acidic foods like citrus fruits and tomatoes commonly trigger flare-ups in sensitive individuals.
Processed foods high in sugar and unhealthy fats can promote inflammation throughout your body, including your prostate gland. A diet lacking in anti-inflammatory nutrients may also fail to provide the building blocks your body needs for healing.
Sedentary Lifestyle Effects
Prolonged sitting, whether at work or during leisure activities, can compress your prostate and restrict blood circulation to the pelvic region. This reduced blood flow limits the delivery of nutrients and oxygen necessary for proper prostate function.
Regular physical activity promotes healthy blood circulation and helps reduce stress hormones that can contribute to inflammation. Men who lead sedentary lifestyles often experience more severe and persistent prostatitis symptoms.
Natural Treatment Approaches That Work
While conventional medical treatments have their place, many men find significant relief through natural approaches that address the root causes of prostatitis. These methods often provide lasting benefits without the side effects associated with long-term medication use.
Dietary Modifications for Healing
Anti-inflammatory foods can significantly reduce prostate inflammation and support your body’s natural healing processes. Omega-3-rich fish like salmon, mackerel, and sardines provide powerful anti-inflammatory compounds that can help calm irritated prostate tissue.

Colorful fruits and vegetables loaded with antioxidants help neutralize free radicals that contribute to inflammation. Berries, leafy greens, and cruciferous vegetables like broccoli and cauliflower should become staples in your daily diet.
Avoiding inflammatory foods is equally important. Limiting refined sugars, processed meats, and excessive alcohol consumption can prevent additional irritation to your already sensitive prostate gland.
Exercise and Physical Therapy
Regular moderate exercise improves blood circulation throughout your pelvic region, delivering essential nutrients to your prostate while removing inflammatory waste products. Activities like walking, swimming, and cycling can provide significant benefits without overexerting your body.

However, avoid activities that place excessive pressure on your perineum, such as long bicycle rides on hard seats or prolonged horseback riding, as these can worsen prostatitis symptoms.
Pelvic Floor Strengthening
Specific exercises targeting your pelvic floor muscles can provide remarkable relief from prostatitis symptoms. These muscles support your bladder and prostate, and strengthening them can improve urinary control and reduce pelvic pain.
Kegel exercises, performed correctly and consistently, can help restore proper muscle function and reduce tension that contributes to prostatitis discomfort. Working with a physical therapist experienced in pelvic floor dysfunction can maximize the benefits of these exercises.
Supplement Solutions for Prostate Health
Evidence-based natural supplements can provide significant support for men dealing with prostatitis. While supplements shouldn’t replace proper medical care, they can enhance your body’s ability to heal and maintain prostate health.

Evidence-Based Natural Compounds
Saw palmetto extract has demonstrated promising results in clinical studies for reducing prostate inflammation and improving urinary symptoms. This palm fruit extract appears to work by blocking certain enzymes that contribute to prostate enlargement and inflammation.
You can read more about this supplement here.
Quercetin, a powerful flavonoid found in onions, apples, and berries, possesses strong anti-inflammatory properties that can help calm irritated prostate tissue. Clinical trials have shown that quercetin supplementation can significantly reduce prostatitis symptoms in many men.
Zinc plays a crucial role in prostate health, and many men with prostatitis have been found to have lower zinc levels. This essential mineral supports immune function and helps maintain healthy prostate tissue.
Beta-sitosterol, a plant compound found in various nuts and seeds, has shown effectiveness in improving urinary flow and reducing inflammation associated with prostate conditions.
Dosage and Safety Guidelines
When considering supplements, quality matters more than quantity. Look for products from reputable manufacturers that provide third-party testing results to ensure purity and potency.
Start with conservative doses and monitor your body’s response before increasing intake. Some supplements can interact with medications or have side effects, so consulting with a healthcare provider familiar with natural treatments is advisable.
Remember that supplements work best as part of a comprehensive approach that includes dietary improvements, stress management, and appropriate medical care when needed.
When to Seek Professional Medical Help
While natural approaches can be highly effective, certain situations require immediate professional medical attention. Recognizing these red flag symptoms can prevent serious complications and ensure you receive appropriate care.

Red Flag Symptoms
Fever accompanied by chills and severe pelvic pain may indicate acute bacterial prostatitis, which requires immediate antibiotic treatment. Delaying care for this condition can lead to serious complications, including blood poisoning.
Complete inability to urinate represents a medical emergency that requires immediate attention. This condition, called urinary retention, can cause serious kidney damage if not treated promptly.
Blood in urine or semen, while sometimes related to prostatitis, can also indicate more serious conditions that require professional evaluation and appropriate testing.
Treatment Options Available
Modern medicine offers various treatment options for prostatitis, ranging from antibiotics for bacterial infections to alpha-blockers that help relax prostate muscles and improve urinary flow.
Physical therapy specifically designed for pelvic floor dysfunction has shown excellent results for many men with chronic prostatitis. These specialized therapists can identify muscle imbalances and teach techniques for reducing pelvic tension.
In severe cases, minimally invasive procedures may be recommended to reduce prostate inflammation or remove infected tissue. These treatments are typically reserved for cases that don’t respond to conservative approaches.
Prevention Strategies for Long-Term Health
Preventing prostatitis recurrence requires a proactive approach that addresses the various factors contributing to prostate inflammation. Implementing these strategies can help maintain long-term prostate health and prevent future episodes.
Daily Habits That Protect Your Prostate
Staying adequately hydrated helps flush bacteria and inflammatory substances from your urinary tract. Aim for 8-10 glasses of water daily, but avoid excessive fluid intake before bedtime to minimize nighttime urination.

Regular bathroom habits are crucial – never hold urine for extended periods, as this can promote bacterial growth and increase infection risk. Complete bladder emptying during each urination helps prevent stagnant urine that can harbor bacteria.
Maintaining good hygiene, particularly after bowel movements, prevents bacterial migration from the rectal area to the urinary tract. Proper hygiene practices are simple but effective prevention measures.
Stress Management Techniques
Chronic stress management is essential for preventing prostatitis recurrence. Regular meditation, deep breathing exercises, or yoga can help reduce stress hormones that contribute to inflammation.
Adequate sleep allows your body to repair and regenerate, supporting immune function and reducing inflammation. Aim for 7-9 hours of quality sleep nightly, maintaining consistent sleep and wake times.
Building strong social connections and engaging in enjoyable activities can provide natural stress relief while improving overall quality of life. Don’t underestimate the healing power of laughter and positive relationships.
You can like to read this article about men’s health, here.
Conclusion
Breaking free from prostatitis pain requires a comprehensive understanding of this complex condition and a commitment to addressing its underlying causes. While the journey to healing may seem overwhelming, remember that millions of men have successfully overcome prostatitis and reclaimed their quality of life.
The key lies in combining evidence-based natural approaches with professional medical care when appropriate. By making targeted dietary changes, incorporating stress management techniques, and considering beneficial supplements, you can support your body’s natural healing processes while addressing the root causes of inflammation.
Remember that healing takes time, and progress may come in waves rather than a straight line. Be patient with yourself and celebrate small improvements along the way. With persistence and the right approach, you can overcome prostatitis and enjoy renewed vitality and confidence.
Your prostate health journey is unique, and what works for others may need to be adapted to your specific situation. Stay informed, work with qualified healthcare providers, and never lose hope – relief is possible, and a pain-free future awaits.
Frequently Asked Questions
1. How long does it typically take to recover from prostatitis? Recovery time varies significantly depending on the type of prostatitis and individual factors. Acute bacterial prostatitis may resolve within weeks with proper antibiotic treatment, while chronic forms can take several months to years to fully heal. Consistency with treatment approaches and lifestyle modifications typically leads to faster recovery.
2. Can prostatitis be completely cured, or will it always come back? Many men achieve complete resolution of prostatitis symptoms and never experience recurrence. However, some individuals may have periodic flare-ups, especially if underlying risk factors aren’t addressed. Maintaining healthy lifestyle habits and stress management typically prevents recurrence in most cases.
3. Are there any foods I should completely avoid if I have prostatitis? While individual sensitivities vary, common trigger foods include spicy dishes, excessive caffeine, alcohol, citrus fruits, and processed foods high in sugar. Keep a food diary to identify your personal triggers, as what affects one person may not affect another.
4. Is it safe to exercise when experiencing prostatitis symptoms? Gentle to moderate exercise is generally beneficial for prostatitis, as it improves circulation and reduces stress. However, avoid activities that put direct pressure on the perineum, such as cycling on hard seats or prolonged sitting. Walking, swimming, and light stretching are typically well-tolerated.
5. Can stress really cause prostatitis, or does it just make symptoms worse? Chronic stress can both trigger prostatitis and worsen existing symptoms. Stress compromises immune function, increases muscle tension, and promotes inflammation throughout the body. Managing stress through relaxation techniques, exercise, and lifestyle modifications is an essential component of prostatitis treatment and prevention.